Cervical smear test
The cervical smear is a test that detects abnormal cells in the cervix. The cervix is the entrance to the uterus from the vagina. Detection of abnormal cervical cells and early treatment can prevent cervical cancer.
Most smear tests are normal, but for about 1 in 20 women (5%) the test detects some abnormal changes in the cells of the cervix. Most of these changes are mild and will not lead to cervical cancer, as these cells can return to normal on their own. In some cases, if indicated and treatment is performed, so these abnormal cells cannot turn into cancer.
It is possible for sexually active women of all ages to develop cervical cancer, although it is more common in women aged 25 to 29 and very rare in women under 25. Although cervical screening is not 100% accurate and does not prevent all cases of cervical cancer, it is the best method for detecting any abnormal cells that could later turn into cancer, therefore regular follow up is important.
The cervical screening programme
The goal of the Cervical Cancer Screening Program is to reduce the number of women who develop cervical cancer and the number of women who die from it. In many national health systems, such as the United Kingdom, screening was introduced in the 1980s, and since then the number of cervical cancers has dropped by about 7% each year.
All women in the United Kingdom are invited to have cervical screening:
- age 25 to 49 years old – every 3 years
- age 50 to 64 years old – every 5 years
- over 65 years – only women who have recently had abnormal results
The smear test can be done during your menstrual cycle (usually 14 days after the start of your last period), as this can ensure a better cell sample. Spermicides and lubricating gels should be avoided for 24 hours before the test, as the chemicals they contain may affect the results.
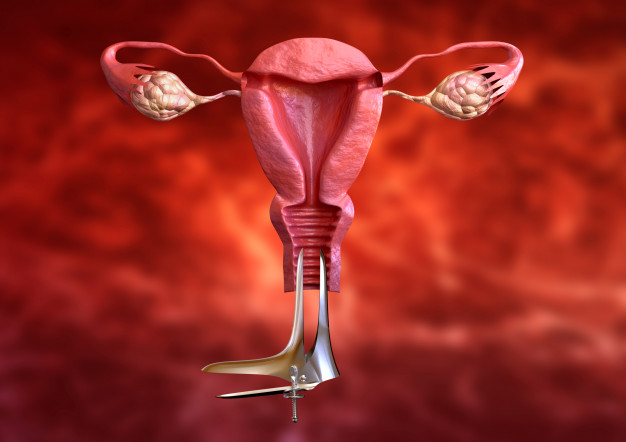
The examination of the cervix usually takes about 5 minutes and to perform, a vaginal speculum is inserted into the vagina, which is an instrument that keeps the walls of the vagina open so that the cervix is visible. The collection of cells from the surface of the cervix is done with a soft brush. Some women find the procedure a little uncomfortable, but for most women it is not painful. The cell sample is then sent to a cytology lab and you should receive the result within 1-2 weeks.
What causes abnormal cervical cells?
Abnormal changes of the cervical cells can be caused by certain types of high-risk human papillomavirus (HPV). HPV is the name of a family of common viruses that affect the skin and mucous membranes, such as those in the cervix, anus, mouth and throat. It is estimated that in many countries, 8 out of 10 people become infected with HPV at some point in their lives. For most people, the virus goes away without treatment and does not cause harm, but for some, infection with certain types of HPV can cause abnormal cell growth, which can lead to the development of cervical cancer.
High-risk types of HPV that can cause abnormalities in the cells of your cervix are transmitted through any skin-to-skin contact with the genital area. This includes vaginal, anal and oral sex and the use of sex toys. Because most types of HPV, including high-risk types, cause no symptoms, you or your partner could have the virus for months or years without knowing it.
How often are the abnormal results?
For every 100 women who have a cervical smear test, about 6 will have an abnormal result. It is very rare (less than 1 in 2,000) to be diagnosed with cancer by the results of a cervical screening test.
Disadvantages of smear test
Although cervical screening can help towards the prevention of cervical cancer, there are some potential disadvantages associated with it. These include:
- Possible discomfort, embarrassment or (less often) pain during the test.
- Incorrect results, which could lead to non-detection of precancerous cells or unnecessary treatment.
Some treatments used to remove pre-cancerous cells may increase the risk of preterm labour (before the 37th week of pregnancy) if you become pregnant in the future.
Women who are not sexually active
The risk of cervical cancer is very low in women who have never had any skin-to-skin contact with the genitals of either a man or a woman. Because the risk is so low, women in this group may choose not to have a smear test.
Cervical smear and HPV vaccination
It is important to get your cervical smear done even if you have been vaccinated against HPV. The vaccine protects you from infection with the HPV viruses (types 16 and 18) that are responsible for most cases of cervical cancer. However, HPV vaccine does not provide protection against all high risk types of the virus; although it significantly reduces the chance of getting cervical cancer, but it does not completely eliminate it.
Cervical smear during pregnancy
Cervical smear is not usually recommended during pregnancy, unless you have missed previous appointments or have had abnormal results in the past.
If you are pregnant and all previous test results were normal, it is usually recommended that you wait up to 3 months after giving birth for your test.
Women aged 65 and over
Women aged 65 and over whose last three results were negative do not need further smear tests. This is because it is very unlikely that women in this group will develop cervical cancer.
If you are over 64 years old and have had abnormal results, you should continue having smear tests until the cells return to normal.
Women who have had a hysterectomy
In women who have undergone a total hysterectomy (removal of the uterus and cervix) the smear test is necessary.
Women who have had a hysterectomy that has left all or part of the cervix should be screened after the end of postoperative care.
Women who have had a total hysterectomy to treat cancer or because of abnormal changes in the cervical cells at the time of the total hysterectomy, need to have cells (vault smear) taken from the vaginal cavity (where the cervix was).
Why is cervical smear not recommended for women under 25?
Women under the age of 25 are not usually invited for a screening as part of the Screening Programme because of the following reasons:
- Cervical cancer is very rare in women under 25
- HPV infection is very common in women under the age of 25 and the immune system often clears the infection and the abnormal cells will return to normal without treatment.
- The number of younger women diagnosed with cervical cancer is likely to decrease due to the HPV vaccination programme.
If you are under the age of 25 and have symptoms of cervical cancer, or you are concerned about the risk of developing cervical cancer or other aspects of your sexual health, you seek advice from your gynaecologist.