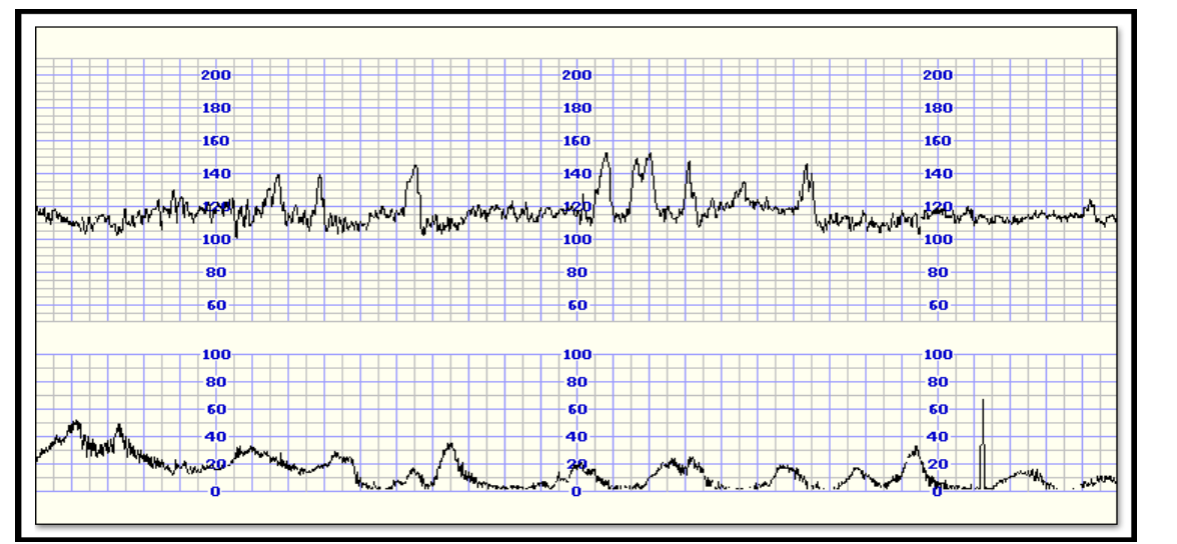
The condition of the fetus is monitored by checking its cardiac function, which is performed by listening to the fetal heart rate with a special ultrasound device intermittently or, and most accurately, by continuous monitoring during labour. The recording of fetal heart is monitored in association of its changes alongside with uterine contractions. The CTG monitor achieved by placing the ultrasound probe the hearing point of the fetal heart rate in the abdominal wall of themmother-external cardiotocography- or by applying a special electrode to the scalp (head) of the fetus (internal cardiotocography). The main parameters of the CTG being evaluated are:
1.Basic fetal rhythm (baseline)
2.Variability of the basic heart rate
3.Transient changes in the heart rate(accelerations, decelerations).
Fetal heart rate naturally ranges from 110 to160 pulses/min and must be kept relatively stable during childbirth. Fetal tachycardia (frequency >170 beats/min) may be caused by tachycardia of the mother due to pyrexia, dehydration or due to fetal hypoxia. If it is significant and persists, it may be due to prolonged fetal hypoxia or congenital heart abnormalities of the fetus. The second parameter evaluated, the variability of the heart rate, expresses the balance of the sympathetic and parasympathetic system. Normal, variability ranges between 10-25 pulses/min. Reduced variability may be due to maternal medications such as diamorphine in labour or because of fetal hypoxia. Normally, reduced variability can also be observed in the sleep phase of the fetus.
Transient changes in heart rate are distinguished in accelerations and decelerations. The presence of accelerations with fetal movements is a normal finding. Absence of accelerations for more than 45 min is considered a pathological finding and should be investigated. Decelerations are classified in early, late and variables. Early decelerations coincide with the contractions as a consequence of the fetal head pressure and are not of clinical importance.
Late decelerations appear with a time delay in relation to the start of the contraction and they are considered a pathological finding; they occur due to fetal hypoxia and placental insufficiency. The variable decelerations are not combined in time with the contractions and they are associated with the pressure of umbilical cord; they are not of particular clinical importance.
Overall, the CTG provides an idea of how well the baby copes in labour. Fetal hypoxia could be checked with more accuracy with fetal blood sampling; the latter means that the obstetrician could take a small amount of blood from baby’s head to obtain the oxygen levels of the baby (pH and base excess).
Fetal pH equals to 7.20-7.25 is a starting point for metabolic acidosis, while pH < 7.20 indicates significant metabolic acidosis. Both CTG findings and fetal sampling results should be taken into consideration with the overall clinical picture and labour progress in order to make the right decisions on individual basis.